Accurate verification of insurance benefits plays a crucial role in managing, Revenue Cycle Management (RCM) and as healthcare providers navigate the complexities of healthcare finance, understanding and implementing effective strategies for insurance benefits verification become imperative. By doing so, providers can optimize their revenue cycle management and enhance patient satisfaction and financial transparency, ensuring a sustainable future in an ever-evolving healthcare background.
Frequently Asked Questions
The business world is being flattened by economics, technology, demographics and regulations. To win in this flattening world, companies must transform their way of working to seek and convert new opportunities wherever those opportunities may be. This means acquiring the ability to disaggregate your operations, people and resources across time zones, geographies, cultures and sourcing and delivering.
1. Why should I outsource to RND Softech?
By outsourcing to RND Softech, you will experience an immediate reduction of up to 60% in your manpower costs. We provide staff to take care of your front end and backend operations. This will enable you to focus on growing your business without having to worry about increasing operational costs, employee attrition, etc.
2. What are the services you offer?
We offer entire Revenue Cycle Management - a few of them being, data entry, insurance verification, authorization, Doctor's office follow-up, intake, order processing, billing, denial management, payment posting, inbound and outbound patient calling, 24 x 7 customer support, scheduling processes etc.
3. Do you have experience of working in the healthcare industry?
Yes, we have more than 22 years of experience working in the US healthcare industry. We have been providing medical transcription services to hospitals across the United States since 1999 and DME/Home care back office services since 2012.
4. What is your on-boarding period for a new employee/customer?
Anywhere between 1 to 14 days.
5. What would be the FTE's working hours?
The FTE would work the US working hours, in the time zone of your choice.
6. Is the contract obligatory? Is there a minimum or maximum contract period?
Yes, but it is a no-obligations contract and is non-binding and there is no minimum contract period. The contract simply states that the two companies are entering into a partnership for the providing and receiving services. You can terminate the contract if you are not satisfied with the services. A notice period of 1 month is appreciated but not mandatory.
7. Are you HIPAA compliant?
Yes, we are certified for HIPAA and Information Security Management Systems.
8. Is there any contract to be signed before getting started?
No, the contract is not obligatory and there is no minimum contract period. The contract simply states that the two companies are entering into a partnership for the providing and receiving services. You can terminate the contract if you are not satisfied with the services. A notice period of 1 month is appreciated but not mandatory.
9. Do you follow FTE based billing or percentage of revenue generated billing?
We follow an FTE-based billing. One FTE (full time employee) works 8 hours a day, 5 days a week - a total of 40 hours a week.
10. How will I be billed?
You will be sent an invoice each month mentioning the number of FTEs agreed upon and the services provided.
11. How can I make payments?
You can make payments through PayPal using your credit card or make a wire transfer.
12. Are the FTEs your own employees or do you subcontract to other smaller companies?
All our FTEs are employees of RND Softech and are dedicated to each client, the agent will not be shared with other clients
13. Where are you located?
We are located in Southern part of India.
14. Do you follow US holidays or local?
Yes, We follow US holidays.
15. Are You Certified?
Yes we are one ISO 9001, ISO 27001, HIPPA and SOC2 Certificates.
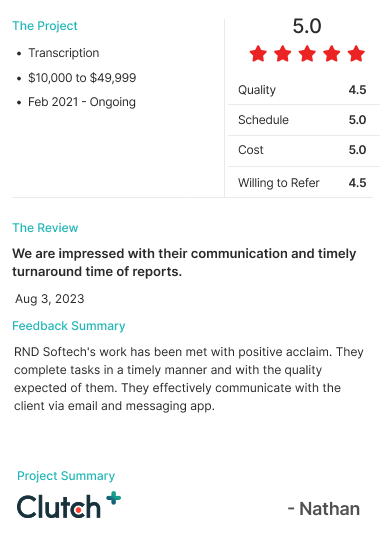
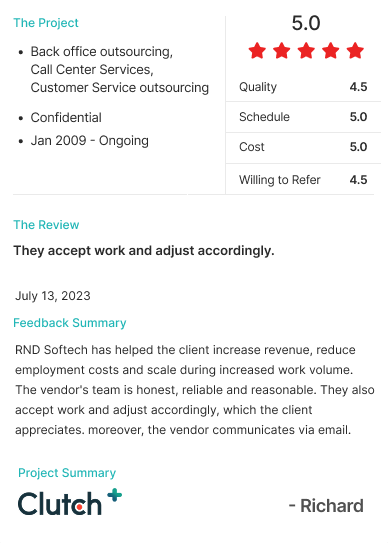
Our
TESTIMONIALS

Certifications
RND Softech, is a 25 year old Pioneer Off-shore BPO staffing partner servicing the US , UK, Canada & Australian markets across 15+ Back office support domains.